Welcome to the Medical Physics FAQ page – hopefully this page will answer any technical questions or concerns you may have about the technology / equipment that will be used to deliver your personalised radiation therapy cancer treatment. If you have any further questions, or if you would like to organise an appointment with one of our friendly Medical Physics team, please email Icon Physics Team and someone will be in touch to arrange an appointment
Medical Physics FAQ
Some of our most Frequently Asked Questions.
Safety and Quality AssuranceSafety and Quality Assurance
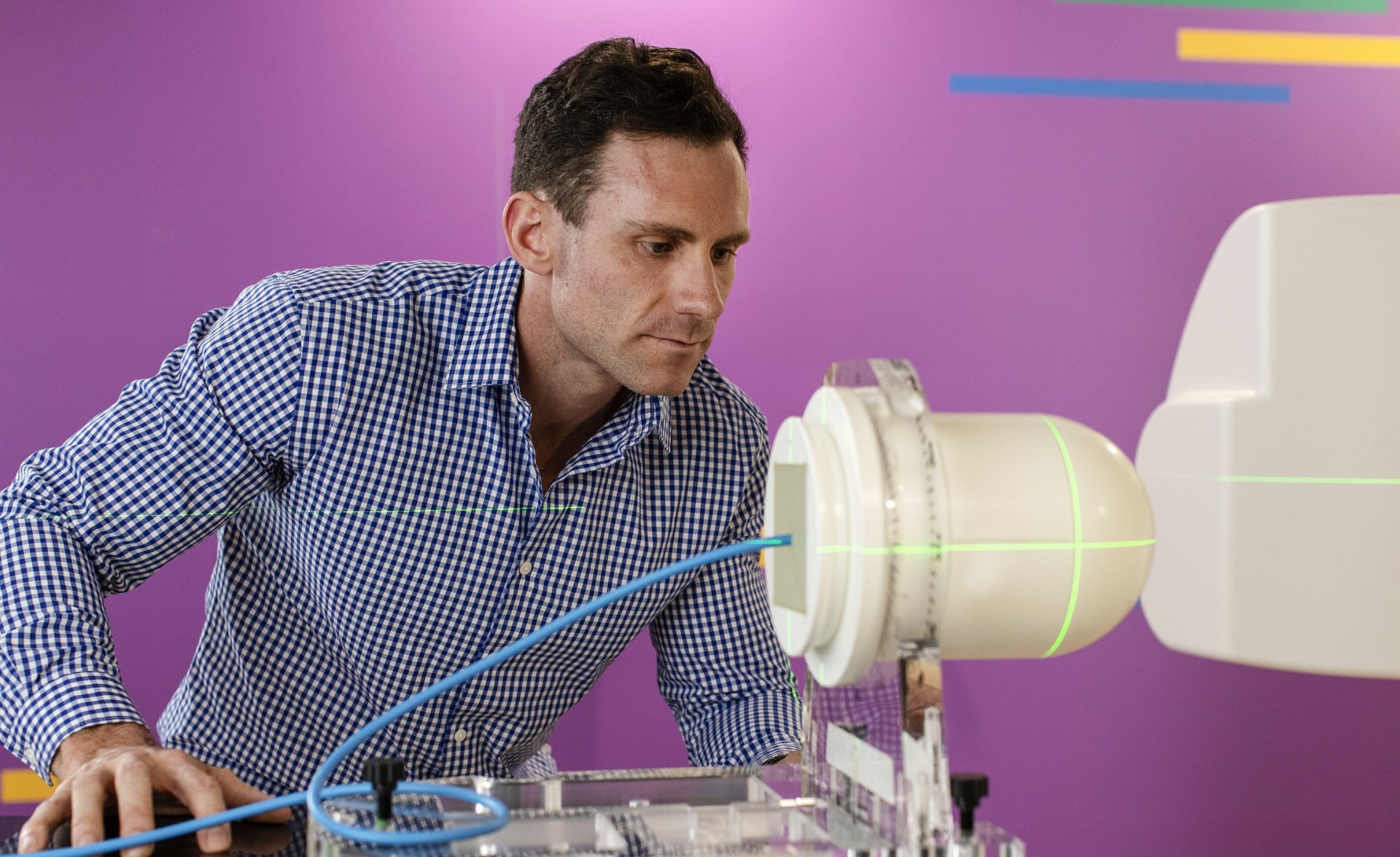
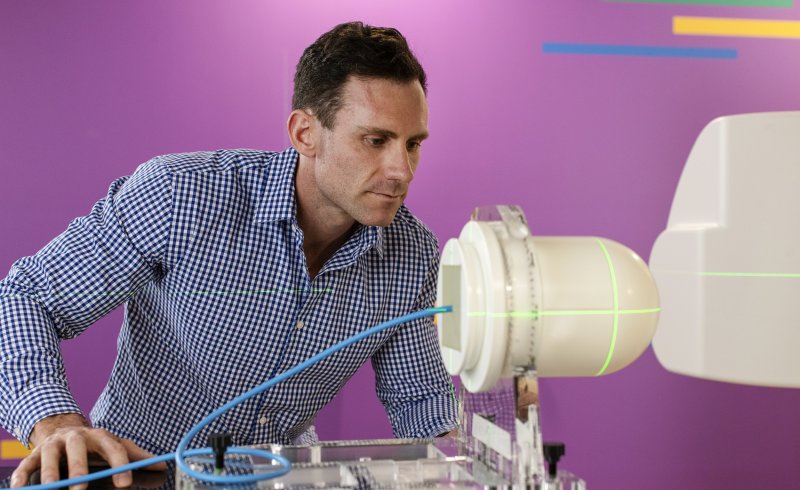
A linear accelerator uses microwave technology to accelerate electrons down a ‘waveguide’. The electrons are then used for an electron treatment or collided into an ‘x-ray target’ to produce high-energy x-rays. These high-energy electrons and x-rays are then shaped as they exit the machine to match the tumour’s shape. The above diagram is a very simplified version – beneath the covers, a linear accelerator looks more like this:
It contains hundreds of electrical and mechanical parts made up of thousands of components that are held together by hundreds of thousands of fixings!
They all work together to create and shape the beam and provide the motions necessary to position you correctly, take the x-ray images that will be used to verify your positioning, and monitor your treatment as it is delivered. The end result is a highly complicated and very precisely delivered beam.
Medical radiation is highly regulated in Australia and New Zealand. One of the medical physicist’s roles is to coordinate a rigorous testing routine that ensures every part of the linear accelerator functions as it should. This includes daily, monthly and annual checks that the beam is being delivered correctly. Icon also participates in national audit programs that provide regular independent verification and monitoring of the radiation beams on every machine.
Your treatment is monitored and checked from start to finish. When you are set up on the machine for treatment each day, the radiation therapist will use various methods – including x-ray imaging – to ensure you are set up correctly and verify that the correct treatment is being delivered on the correct day. While your treatment is being delivered, the machine itself is monitoring its own delivery, and the radiotherapists will be watching you on closed circuit cameras to make sure you are OK. There are also microphones so that they can talk to you, and you can call out if you need their attention. After your treatment is delivered, the machine records everything, including all the images taken, back to your permanent treatment record. An independent radiotherapist who wasn’t involved in your treatment reviews each record for further quality assurance purposes.
Accidents in radiotherapy are extremely rare. This is because of the rigorous program of system quality assurance and maintenance, as well as the number of checks that are put into place throughout every part of your treatment process. If something does occur that might impact your treatment, there are globally established methods to account for this, and you will be kept informed of what is happening. Sometimes a problem with the linear accelerator might interrupt your treatment – if this happens, the medical physicist and perhaps a specialist engineer will restore the machine to service as quickly as possible. Then the medical physicist will carry out all the appropriate checks to ensure it is ready to be put back into clinical use.
Every day before treatment can start, a radiotherapist or a medical physicist runs the linear accelerator through a series of tests that are designed to ensure the machine is performing safely and to specification. Medical physicists also carry out an in-depth program of quality assurance checks on a weekly, monthly and annual basis. This program is based on an international standard that has been established by medical physicists all over the world. In addition, specialist engineers regularly perform their own maintenance and inspection programs that monitor the internal functioning of the machine.
Your treatment plan is unique to you, and it has been devised by a whole team of people. Your radiation oncologist and a planning radiotherapist work together to create the right plan for your treatment. Sometimes a medical physicist, another planner or another RO may be called in to advise on a particular component of the plan. When the plan is completed, it is checked by an independent planning radiotherapist – someone who was not involved in the original work. It is also run through a series of checks by the medical physicist to ensure that it is correct.
Treatment Planning and DeliveryTreatment Planning and Delivery
The type of radiation you will receive will depend on the size and location of your lesion(s) or target volume(s) of your treatment. There are two treatment techniques you could undergo: External Beam Radiotherapy (EBRT) or Internal Radiation Therapy (IRT), more specifically, Brachytherapy.
EBRT is by far the more common technique, and the types of radiation used are:
- High energy x-rays: this is the majority of EBRT and is usually prescribed for deep-seated tumours and/or those that are close to healthy organs and tissues.
- High energy electrons: this makes up a smaller proportion of EBRT and is often used for superficial/shallow tumours that are not too far below the skin.
- Medium energy x-rays: also called superficial x-rays or orthovoltage x-rays; these are less penetrative than higher energy radiation and are used for skin cancers.
Brachytherapy treatments are less commonly available, and they use sealed radioactive sources that are inserted in the patient either temporarily or permanently. The type of radiation these radioactive sources produce is typically gamma radiation.
Yes! Each patient undergoing radiotherapy gets a treatment plan formulated uniquely just for them. Your treatment plan is tailored specifically to you, accounting for the type, location, size, extent, and spread of your disease. The plan would also consider the dose to surrounding organs and tissues, any implantable devices or prostheses you may have, as well as your treatment history and other medical procedures you have undergone or undergoing.
Typically, the process starts with the Radiation Oncologist (RO) prescribing the treatment by stipulating the dose of radiation to the target region/organ. Next, you would be booked in for a ‘simulation scan’ session; the Radiation Therapists (RTs) will scan the region of your body containing the target region(s), or volume(s), using an x-ray CT. Your scan is then sent to the RO, who marks the target volumes on your scan (like marking an area on a map!), confirming the prescription and also adding constraints to the dose allowed to surrounding healthy tissues and organs.
The RTs then begin creating your unique treatment plan and may consult the RO and the Medical Physicist (MP) along the way. The plan is created and calculated using a treatment planning system (TPS) on a computer. Once an optimum plan is produced, it is reviewed and approved by the RO and then checked by the MP, who also performs quality assurance (QA) checks and measurements to ensure the plan matches the intent of the treatment. When all these steps are completed successfully, independent RTs check that all required checks, QA, reviews and assessments are completed before readying for treatment.
The radiation is targeted to your tumour, but depending on the tumour location, the radiation beam or ray will typically traverse through other tissues before reaching the tumour. To concentrate the radiation where it is needed (in the tumour) while avoiding healthy tissues and organs as much as possible, the radiation source will deliver the beam from multiple directions. The radiation beams will intersect and therefore concentrate the dose in the tumour while minimising the dose in surrounding tissues.
General Radiation Question / ConcernsGeneral Radiation Question / Concerns
Yes! Radiation can be found in your everyday life in many forms. For more information on background radiation, ANSTO provides great resources:
https://www.ansto.gov.au/education/nuclear-facts/what-is-radiation
In some cases, radiation exposure can, after a long period of time, cause cancer. However, the radiation we use during treatment is very targeted to your individual tumour to minimise this risk as much as possible. If you are concerned, you should discuss the risks and benefits with your Radiation Oncologist
Radiation damages the DNA in tissue, which is why we tailor your treatment to target only the malignant tissue. Normal tissue can repair itself from radiation exposure, whereas tumour cells cannot.
Cells within the body constantly go through a life cycle involving cell death. The body is designed to break down and dispose of the resultant cell fragments; the same is true of tumour cells after they die.
About Icon Group
Icon Group is Australia’s largest dedicated cancer care provider and has expanded globally into Singapore, Mainland China, Hong Kong and New Zealand.
Our people
People from across Icon Group share their stories of success, career progression and being iconic.
A career with Icon
At Icon, you’ll help change lives, every single day. In return for your passion, dedication and agility, we offer a workplace where you can.
Updates
Read the latest news and updates across Icon Group.